Pain is something everyone experiences but not all pain is the same. If you’ve ever pulled a muscle during a workout or dealt with lingering back pain for months, you’ve experienced two very different types of discomfort. Understanding the difference between acute vs chronic pain isn’t just helpful it’s essential for getting the right treatment and protecting your long-term health.
Acute pain usually appears suddenly and fades as your body heals. Chronic pain, on the other hand, sticks around much longer and can continue even after an injury has resolved. The distinction affects how doctors diagnose, treat, and manage pain.
If you’re unsure about how pain medications actually work, you may also want to review some of the common myths about painkillers that often lead to confusion about treatment options.
In this guide, we’ll break down the key differences between acute and chronic pain in a clear, straightforward way so you can better understand what your body may be telling you.
Contents
- 1 What Is Acute Pain?
- 2 What Is Chronic Pain?
- 3 Acute vs Chronic Pain: Side-by-Side Comparison
- 4 Causes of Acute Pain
- 5 Causes of Chronic Pain
- 6 How Treatment Differs Between Acute and Chronic Pain
- 7 Can Acute Pain Turn Into Chronic Pain?
- 8 Emotional and Mental Health Impact
- 9 When Should You See a Doctor?
- 10 Why Understanding the Difference Matters
- 11 Frequently Asked Questions
- 12 Final Thoughts
What Is Acute Pain?
Acute pain is short-term pain that typically lasts less than three months. It usually starts suddenly and is directly linked to a specific injury, illness, or medical condition.
Acute pain acts as the body’s warning system. According to Mayo Clinic, it typically resolves once the underlying cause is treated.
Think of acute pain as your body’s built-in alarm system. It alerts you that something is wrong and needs attention.
Common Examples of Acute Pain:
- Sprained ankle
- Broken bone
- Burn or cut
- Post-surgical pain
- Dental pain
- Infection-related pain
Key Characteristics of Acute Pain:
- Sudden onset
- Sharp or intense sensation
- Clearly identifiable cause
- Improves as the injury heals
- Temporary
Acute pain serves an important protective purpose. For example, if you touch a hot stove, the sharp pain makes you pull your hand away immediately. Without that signal, further injury could occur.
Most acute pain resolves once the underlying issue heals. If it continues beyond the expected recovery period, it may require medical evaluation.
What Is Chronic Pain?
Chronic pain is pain that lasts longer than three months or beyond normal healing time. Unlike acute pain, chronic pain does not always serve a protective function. In many cases, it continues even after the original injury or illness has resolved.
Chronic pain can be constant or come and go. It may feel dull, aching, burning, throbbing, or even sharp at times.
For a deeper look at structured treatment approaches, read our guide on managing chronic pain safely, which explains medication use, lifestyle adjustments, and alternative therapies.
Common Causes of Chronic Pain:
- Arthritis
- Chronic back pain
- Nerve damage (neuropathy)
- Fibromyalgia
- Migraines
- Autoimmune conditions
Key Characteristics of Chronic Pain:
- Lasts 3+ months
- May not have a clear cause
- Can persist after healing
- Often affects mood and sleep
- May require long-term management
Chronic pain doesn’t just affect the body it can impact emotional well-being, work performance, relationships, and overall quality of life. It’s often associated with anxiety, depression, and sleep disturbances.
Also Read: Tapentadol for Post-Surgical Pain: How Safe & Effective Is It?
Acute vs Chronic Pain: Side-by-Side Comparison
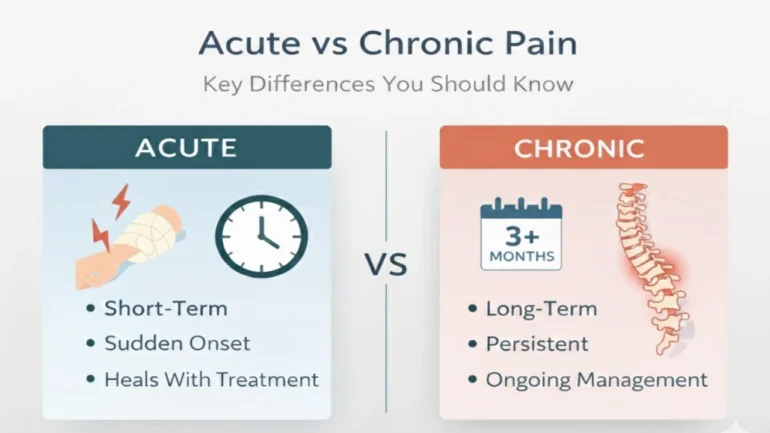
Here’s a clear breakdown of the difference between acute and chronic pain:
| Feature | Acute Pain | Chronic Pain |
|---|---|---|
| Duration | Short-term (less than 3 months) | Long-term (3+ months) |
| Onset | Sudden | Gradual or ongoing |
| Cause | Injury, illness, surgery | Ongoing condition or nerve changes |
| Purpose | Protective warning signal | Often no protective purpose |
| Emotional Impact | Temporary stress | Anxiety, depression possible |
| Treatment | Short-term relief | Long-term management plan |
Understanding these differences helps guide appropriate treatment decisions.
Causes of Acute Pain
Acute pain is usually triggered by a specific event or injury.
Physical Injuries
Falls, sports injuries, and accidents commonly cause acute pain. Muscle strains and fractures are classic examples.
Surgical Procedures
Post-operative pain is expected and typically improves with recovery.
Illness or Infection
Conditions like appendicitis, strep throat, or kidney stones can cause sudden, intense pain.
Burns or Cuts
Damage to tissues activates nerve endings, causing immediate pain signals.
Acute pain typically improves as inflammation decreases and tissues repair.
Causes of Chronic Pain
Chronic pain often develops differently and may involve changes in the nervous system.
Long-Term Conditions
Arthritis, spinal disorders, and autoimmune diseases commonly lead to persistent pain.
Nerve Damage
In some cases, nerves continue sending pain signals even after tissues have healed.
Past Injuries
Sometimes acute pain evolves into chronic pain if healing is incomplete or nerve sensitivity increases.
Unknown Causes
In certain cases, the original cause of chronic pain cannot be clearly identified.
Chronic pain is often more complex than acute pain and may require a comprehensive management strategy.
How Treatment Differs Between Acute and Chronic Pain
Treatment approaches vary significantly depending on whether pain is acute or chronic.
Treating Acute Pain
The focus is on addressing the cause and reducing inflammation.
Common approaches include:
- Rest
- Ice or heat therapy
- Short-term medication
- Physical therapy (if needed)
- Recovery-focused care
The goal is to allow the body to heal while minimizing discomfort.
Treating Chronic Pain
Chronic pain management often requires a long-term, multi-layered approach.
Treatment may include:
- Ongoing pain management plans
- Physical therapy
- Exercise programs
- Stress reduction techniques
- Behavioral therapy
- Lifestyle adjustments
- Sleep optimization
Because chronic pain affects both physical and emotional health, treatment often involves a multidisciplinary strategy.
Can Acute Pain Turn Into Chronic Pain?
Yes, in some cases, acute pain can develop into chronic pain.
This may happen if:
- An injury doesn’t heal properly
- Nerve damage occurs
- Pain is not adequately managed
- Inflammation persists
- There is repeated strain or reinjury
Early and appropriate treatment of acute pain reduces the risk of it becoming chronic.
Emotional and Mental Health Impact
Chronic pain isn’t just physical it affects mental health as well.
People living with long-term pain may experience:
- Depression
- Anxiety
- Irritability
- Sleep problems
- Reduced motivation
Pain and stress can create a cycle where each worsens the other. Addressing emotional health is an important part of managing chronic pain effectively.
When Should You See a Doctor?
You should consider medical evaluation if:
- Pain lasts longer than expected
- Pain worsens over time
- You experience numbness or weakness
- Pain interferes with daily activities
- Sleep is consistently disrupted
- You need increasing amounts of medication for relief
Persistent pain should never be ignored. Early assessment can prevent complications and improve long-term outcomes.
Why Understanding the Difference Matters
Knowing whether you’re dealing with acute or chronic pain helps:
- Determine proper treatment
- Prevent unnecessary medication use
- Reduce risk of long-term complications
- Improve quality of life
- Set realistic recovery expectations
Misunderstanding pain types can delay proper care and prolong suffering.
Frequently Asked Questions
Acute pain typically lasts less than three months and resolves as the underlying injury or illness heals.
Some causes of chronic pain can be treated, but many cases require ongoing management rather than complete elimination.
The primary difference is duration. Acute pain is short-term and linked to a clear cause, while chronic pain lasts longer than three months and may persist even after healing.
Yes. Stress can heighten pain sensitivity and increase inflammation, making symptoms feel more intense.
Not always. In some cases, chronic pain continues without a clearly identifiable source.
Final Thoughts
Understanding the difference between acute vs chronic pain is key to making informed decisions about your health. Acute pain is usually temporary and protective, while chronic pain often requires long-term management and a broader treatment approach.
If pain persists beyond normal healing time or significantly impacts your daily life, seeking medical guidance is essential. Early intervention can improve outcomes and help prevent complications.
Pain is your body’s way of communicating. Learning how to interpret that message can empower you to take control of your health and well-being.
Also Read: Buy Tapentadol Online: Certified USA Pharmacy Delivery